Addiction specialist Julia Arnsten, M.D., M.P.H., is frustrated.“You’d think that by now, thousands of years after healers began using cannabis, we’d have more answers about its medicinal value,” says Dr. Arnsten, chief of the division of general internal medicine at Einstein and Montefiore and professor of medicine, of epidemiology & population health, and of psychiatry and behavioral sciences at Einstein.
In 2016, after New York State legalized cannabis for medical use, Dr. Arnsten began looking for safer alternatives to opioids for the one in five American adults suffering from chronic pain. Medical cannabis—offering pain relief with far less potential for abuse compared with opioids—seemed to fit the bill. Yet conducting research with cannabis was, and still is, rife with legal and regulatory hurdles. (See the glossary below for the difference between cannabis and marijuana.) “Our goal here is pain relief,” says Dr. Arnsten, distilling her work down to its essence. “We’re just trying to demonstrate safety and efficacy.”

Our goal here is pain relief. We’re just trying to demonstrate safety and efficacy.
—Dr. Julia Arnsten
She is among a group of Einstein and Montefiore researchers investigating the potential of cannabis for treating various types of pain as well as autism spectrum disorders and other conditions. They’re also working to educate patients about the risks and benefits of medical cannabis, reduce disparities in access to the drug, and establish clinical guidelines for its use.
The need is urgent: Although federal law still prohibits the use of cannabis, all but three states (see the map below) have now legalized it in some form—and its use is increasing, with nearly one in five Americans having tried cannabis at least once during 2019, according to the U.S. Centers for Disease Control and Prevention. But like all drugs, cannabis can cause adverse effects, such as cannabis-use disorder (see below). Ideally, Einstein and Montefiore’s medical-cannabis research will help reveal both benefits and risks.
Cannabinoids:
A class of compounds, found in the cannabis plant as well as humans and other animals, that bind to certain nerve-cell receptors.
Cannabis:
Any plant of the genus Cannabis with leaves and flowering tops having intoxicating effects as well as psychoactive effects in the brain that can alter perception, mood, cognition, and behavior.
Cannabis-use disorder:
The inability to stop using cannabis even if it’s causing health and social problems. A 2015 survey published in JAMA Psychiatry found that approximately three in 10 cannabis users have the disorder. Long-term or frequent cannabis use has also been linked to increased risk of psychosis or schizophrenia in some users.
Endocannabinoids:
Cannabinoids naturally produced by our bodies.
Hashish:
Concentrated resin made from the flowering buds of female cannabis plants, which produces a more-potent high than marijuana.
Hemp:
A variety of cannabis cultivated for its fiber, edible seeds, and oils, usually containing very low levels of THC. Hemp is legal in the U.S.
Marijuana (a.k.a. weed, pot, Mary Jane):
While often used interchangeably with cannabis, these terms refer more specifically to those parts of the plant that, when smoked or swallowed, make you feel high.
Medical cannabis or medical marijuana:
Derivatives of the cannabis plant that are used to ease symptoms caused by certain medical conditions.
Phytocannabinoids:
Any of the 100 or so compounds found in the cannabis plant, including:
Cannabidiol (CBD) and Cannabidivarin (CBDV): Two chemically similar cannabis ingredients that have psychoactive properties but don’t produce a high. CBD, the second most common cannabis ingredient after THC, is widely sold for treating conditions such as pain, anxiety, inflammation, and insomnia. Under federal law, U.S. consumers can purchase CBD and CBDV products as long as they are hemp derived and contain only trace levels of THC.
Tetrahydrocannabinol (THC): The primary psychoactive ingredient of cannabis, responsible for making people feel high.
“Over the years, I’ve had a lot of patients who’ve told me that cannabis helped alleviate their pain, and they wanted something other than opioids,” Dr. Arnsten says. “But even after medical cannabis was legalized in New York, I didn’t want to be just another dispenser, recommending this or that flower to smoke. We knew very little about how to use cannabis or if it worked at all. As practitioners in the field, we weren’t managing it properly.”
In 2017, Dr. Arnsten and colleagues launched the Medical Marijuana and Opioids (MEMO) study—the first long-term investigation into whether cannabis can reduce opioid use among adults with chronic pain; it was recently completed.
The study, funded by the National Institutes of Health (NIH), involved 225 participants with different ailments and varying degrees of opioid use. Based on interim responses on a self-assessment scale, cannabis users reported less pain, greater enjoyment in life, and higher levels of activity, while at the same time noting that they were able to reduce their use of opioids.
Over the years, I’ve had a lot of patients who’ve told me that cannabis helped alleviate their pain, and they wanted something other than opioids.
— Dr. Julia Arnsten
The trial suffered from a major limitation: The researchers had no control over the types of cannabis extract purchased by participants.
Cannabis comes in many forms: It can be smoked or vaped (inhaled) or swallowed in gummies or tinctures; doses can vary, and so can the ratios of active ingredients. To abide by state and federal regulations, however, the researchers were required to send study subjects to licensed state dispensaries, where pharmacists ultimately decided which participants got which formulations, based on clinicians’ recommendations.
Dr. Arnsten hopes to get more data from a randomized, double-blind study called ReLeaf, which is funded by the Laura and John Arnold Foundation and ended in October 2023. Like MEMO, ReLeaf is assessing whether cannabis can reduce opioid use among patients with chronic pain.
But in a clever twist, each of ReLeaf’s 267 participants receives a voucher for purchasing one of four different oral cannabis extracts (including a placebo) at state dispensaries. This novel study design allows the researchers to randomly allocate specific formulations and still comply with regulations. After the participants have undergone 14 weeks of treatment, the researchers measure their cumulative opioid use, pain levels, mental health symptoms, and adverse events.
More typically in recent years, the NIH has favored research into the risks of cannabis rather than into its benefits. An analysis published in 2020 in Science found that the NIH’s National Institute of Drug Abuse—the biggest funder of cannabis research—spent more than $1 billion on cannabis studies between 2000 and 2018. More of those funds went to research into cannabis misuse and adverse effects than to studies of cannabis and cannabis-derived ingredients as therapeutic drugs.
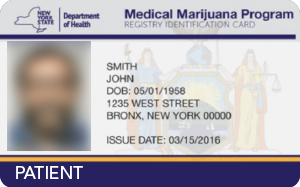
New York’s legalization of medical cannabis in 2016 didn’t guarantee access to the drug. In New York, as in most states, a person must first receive permission (referred to as “certification”) from a practitioner licensed to prescribe controlled substances.
The cost of getting certified (typically $200) is not covered by health insurance, nor is the cost of the cannabis, which can amount to hundreds of dollars a month at a licensed dispensary and must be paid in cash.
“While these costs are affordable for many people, they’re a burden for most of our patients,” says Dr. Arnsten. This means that low-income patients are effectively blocked from obtaining medical cannabis through legal sources. Instead, many must turn to illegal, unregulated dispensaries, where costs are lower but quality and dosages are not controlled.
There are many unsavory practitioners out there who certify patients but don’t spend enough time counseling them about the different types of cannabis, the contraindications, and the risk of adverse events.
— Dr. Julia Arnsten
In 2017, Dr. Arnsten and her colleagues created the Montefiore Medical Cannabis Program (MMCP) to address this new healthcare disparity. The program—the first of its kind in an academic medical center—offers patients free certification to obtain cannabis at licensed pharmacies, along with advice and counseling.
“In academia, we usually wait for drugs to undergo safety and efficacy studies before enabling access to them,” says Dr. Arnsten. “But there are many unsavory practitioners out there who certify patients but don’t spend enough time counseling them about the different types of cannabis, the contraindications, and the risk of adverse events. The way that we’re doing it is safer.”
So far, more than 3,000 patients have participated in the MMCP. Most are seeking relief from chronic pain stemming from degenerative joint disease, inflammatory arthritis, HIV, sickle-cell anemia, fibromyalgia, or neuropathy.
Much more remains to be done to ensure equitable access to medical cannabis, says Dr. Arnsten. She estimates that half the patients certified by MMCP do not end up purchasing the drug at licensed dispensaries, largely because of the expense. Instead, many patronize unregulated dispensaries or continue using prescription opioids, since insurance copays reduce the cost.
“It’s time to advocate for a new federal classification for cannabis so insurance companies can cover it, just as they cover the costs of drugs to treat cancer, diabetes, and other diseases,” Dr. Arnsten recently wrote in STAT, an online healthcare publication.
As of the summer of 2023, New York State had 40 dispensaries offering medical cannabis for sale, with just one in the Bronx. New York State approved cannabis for recreational use in 2021; 23 licensed and regulated dispensaries for selling recreational cannabis have opened so far, two of them in the Bronx.
Anyone who thinks medical-cannabis users are just looking to get high should talk to “Connie” (not her real name), a young woman from Rockland County, N.Y., who is a patient of Julia Arnsten, M.D.
Fourteen years ago, Connie crashed while riding an all-terrain vehicle, smashing a cervical vertebra and breaking her nose. The accident left her with chronic neck pain, periodic migraines, and debilitating anxiety. Physical therapy, yoga, weight training, and Botox injections offered some relief. But even though her symptoms persisted, she insisted on avoiding prescription painkillers.
“They make me sick,” she says. “And I grew up in a town where it seemed everyone was abusing oxycodone and getting hooked on heroin.” Instead, she began experimenting with street marijuana. Smoking weed provided modest relief, and she became a regular user.
I know some people think it leads to heavier drugs. But I can tell you it never made me want to do that.
— “Connie”
Years later, Connie’s mom, then a Montefiore employee, told her about the medical center’s new medical-cannabis program, where patients can get counseling about the plant’s therapeutic uses and, if appropriate, a certificate for obtaining cannabis at licensed pharmacies. Connie got her certificate after consulting Dr. Arnsten, one of the program’s founders and chief of the division of general internal medicine at Einstein and Montefiore.
Medical cannabis eased Connie’s pain and migraines, significantly improving her quality of life. “It also helped me relax and get a good night’s sleep,” she adds. She used the drug as she recovered from two operations without having to resort to conventional pain meds.
Connie soon realized that it was better to buy cannabis from a licensed provider than from a dealer. “When you’re buying it illegally, you don’t know what you’re getting, or what strains might be best for you. For example, I learned that sativa [one of the two main strains of cannabis] can actually trigger anxiety,” says Connie, who spends $200 to $300 a month on the drug.
Connie admits that medical cannabis—which she smokes, vapes, or eats depending on her symptoms—can get her high if she takes too much. But that’s an unwanted side effect, not the goal. She makes a point of not taking cannabis before she goes to work or gets behind the wheel, just in case it impairs her faculties.
“I’m a big advocate of medical marijuana,” says Connie, now an administrative assistant at Montefiore. “I know some people think it leads to heavier drugs. But I can tell you it never made me want to do that. At most, it made me want to get hamburgers or pizza and sit down in front of the TV.”
The MMCP provides a reliable source of information about medical marijuana for residents of the Bronx and surrounding communities. But such expertise can be difficult to find elsewhere in the city and state.
Surveys have shown that most physicians nationwide have little practical knowledge of medical cannabis, a topic rarely covered in medical schools or residency programs. In New York State, just 3 percent of physicians have registered as medical-cannabis providers.
It certainly doesn’t help that some major professional organizations, such as the American Medical Association, still advise against using medical cannabis. Others, including the American Academy of Family Physicians, recommend a more-nuanced approach in which patients are carefully evaluated by appropriate providers. Adding to this muddle, federal authorities still classify cannabis as a schedule 1 substance—saying, in essence, that it’s no more medically useful than cocaine or heroin, and just as dangerous.
To fill this information vacuum, the New York State Department of Health AIDS Institute crafted clinical guidelines for practitioners wishing to know more about medical marijuana. Published in early 2022, Therapeutic Use of Medical Cannabis in New York State provides a comprehensive overview of cannabis pharmacology; the endocannabinoid system (see glossary); the therapeutic uses of cannabis; cannabis formulations; methods of administration, patient assessment, treatment initiation, and patient monitoring; and side effects. The document is available online here. Its lead authors are Dr. Arnsten and Deepika Slawek, M.D., M.S., M.P.H., assistant professor of medicine at Einstein.
Einstein physicians Deepika Slawek, M.D., M.S., M.P.H., and Julia Arnsten, M.D., M.P.H., were the lead authors of Therapeutic Use of Medical Cannabis in New York State. The 28-page guideline was issued in 2022 by the New York State Department of Health AIDS Institute. “Ultimately, patients are using and want to use medical cannabis,” the document says. “It is important to discuss it with them and to encourage safe use of medical cannabis as a harm reduction principle or when other treatment modalities have failed.”
Dr. Slawek, one of Dr. Arnsten’s frequent collaborators, is evaluating cannabis for pain relief with a particular focus on HIV-associated neuropathy—nerve damage that can cause debilitating pain. Neuropathy is a common complication of HIV infection and often a cause of poor HIV outcomes.
“Unfortunately, there’s a dearth of options for these patients, other than opioids and antiepileptic drugs—powerful medications with powerful side effects,” says Dr. Slawek, whose work is funded by the NIH. In her pilot study, the first of its kind, 100 people with HIV will be randomized—using vouchers as in the ReLeaf study—to receive cannabis extracts with different ratios of tetrahydrocannabinol (THC) and cannabidiol (CBD), the plant’s two best-understood and most-common active ingredients.
The study will assess how the extracts affect the patients’ pain, inflammation, and HIV outcomes after 14 weeks of use. These measures may also provide insights into the little-known mechanisms by which cannabis promotes analgesia, or pain relief.

Unfortunately, there’s a dearth of options for patients with HIV-associated neuropathy, other than opioids and antiepileptic drugs.
— Dr. Deepika Slawek
Curing head and neck cancer while preserving speech and swallowing usually requires radiation therapy combined with chemotherapy, which is associated with significant acute side effects. Patients may experience painful sore throats, difficulty swallowing, nausea, and loss of taste, all of which can conspire to decrease appetite and compromise nutrition.
Depending on the level of pain and discomfort, physicians usually prescribe medicated mouthwashes and narcotics, which can lead to problems of their own. The renewed interest in medical cannabis has prompted many oncologists, palliative-care specialists, and patients to ask whether cannabis might be a safer alternative for patients with head and neck cancer, and might also reduce opioid use.

Our patients should not be smoking or vaping cannabis or other substances, which can irritate the throat’s mucosal lining and make everything worse.
— Dr. Rafi Kabarriti
“The short answer is that we need data,” says Rafi Kabarriti, M.D., associate professor of radiation oncology at Einstein and co-director of the NCI-designated Montefiore Einstein Comprehensive Cancer Center’s head and neck cancer team. “There are precious few data to guide us. What we can definitely say is that our patients should not be smoking or vaping cannabis or other substances, which can irritate the throat’s mucosal lining and make everything worse.”
Dr. Kabarriti and his colleagues are conducting a pilot study of 30 adults with head and neck cancer who have received certificates for obtaining different formulations of medical cannabis while undergoing chemotherapy and radiation therapy.
The study’s primary goal is to discover whether patients are able to use the certificates appropriately to obtain and adhere to their cannabis regimens. Funded by Montefiore’s department of radiation oncology, the study will also compare how the different cannabis formulations affect patients’ quality of life, concurrent opiate use, oral microbiomes, appetite, nutritional habits, and weight loss. The researchers will also determine whether age, frailty, and prior use of cannabis influence outcomes.

The Chinese emperor Fu Hsi describes Ma (the Chinese word for cannabis) as a popular medicine possessing both yin and yang.

Cannabis is used in ancient Greece as a remedy for earache, edema, and inflammation.
Jamestown settlers bring marijuana plants to North America.
George Washington grows hemp at Mount Vernon; his ledgers show he has a particular interest in the medicinal use of cannabis.

Cannabis is added to the U.S. Pharmacopeia as a treatment for numerous conditions, including alcoholism and opiate addiction.

Massachusetts becomes the first state to restrict access to cannabis, requiring a doctor’s Rx for purchases from licensed pharmacists. Many other states later enact similar laws.
Responding to a demand for cannabis-based drugs, pharmaceutical companies Eli Lilly and Parke-Davis sell standardized cannabis extracts for pain relief and other uses.
The movie that comes to be known as Reefer Madness debuts, warning of the evils of cannabis use.

Congress includes marijuana in the Narcotics Control Act. A first-offense marijuana possession carries a minimum sentence of 2–10 years with a fine of up to $20,000.

• NORML, the National Organization for the Reform of Marijuana Laws, is founded.
• President Nixon signs the Controlled Substances Act, classifying cannabis as a schedule 1 drug along with heroin and LSD.
National Institute of Mental Health researchers discover cannabinoid receptors present on neurons and some other cells.

California becomes the first state to legalize medical marijuana. Since then, more than 40 states and the District of Columbia have done the same.
New York becomes the 23rd state to legalize medical cannabis. Conditions approved for use include cancer, HIV/AIDS, Parkinson’s disease, and multiple sclerosis.

The FDA approves the first cannabis-based drug, Epidiolex, an oral solution of CBD, for treating seizures associated with two rare and severe forms of epilepsy.

President Joe Biden pardons thousands convicted of possessing cannabis.
Cannabis continues to remain illegal under federal law.
Source: BritannicaProCon.org. Epidiolex Image: Jazz Pharmaceuticals.
Children with autism spectrum disorder (ASD) often exhibit disruptive behaviors and irritability. Treatment for those problems is currently limited to risperidone or aripiprazole, potent drugs that are also prescribed for schizophrenia and bipolar disorder. They can reduce many ASD symptoms—but at the cost of metabolic disorders such as obesity, motor issues, and other serious complications.
Animal studies suggest that phytocannabinoids (naturally occurring compounds in cannabis plants) may be safer for the metabolism of children on the spectrum than other available treatments, says Eric Hollander, M.D., professor of psychiatry and behavioral sciences and director of the autism and obsessive-compulsive spectrum program at Einstein and Montefiore.
In the first clinical trial of its kind, the U.S. Department of Defense is funding an investigation by Dr. Hollander and colleagues to determine whether a phytocannabinoid called cannabidivarin (CBDV) can relieve ASD symptoms without causing harmful side effects. CBDV’s molecular structure closely resembles that of CBD—a popular phytocannabinoid now being sold for conditions ranging from anger to Alzheimer’s. CBD and CBDV are both psychoactive—meaning they can alter mood, perception, and behavior—but they don’t produce a high.

There’s a great need for more controlled clinical trials, both for efficacy and for safety.
—Dr. Eric Hollander
The CBDV clinical trial (expected to be completed by August 2024) involves 100 children, ages 5 to 18, with ASD. They’ll be randomized to receive CBDV or a placebo over 14 weeks. Dr. Hollander’s team is also testing whether CBDV can help individuals with a rare form of autism called Prader-Willi syndrome (PWS), which shares many symptoms with ASD and includes the added complication of compulsive eating.
The body is awash in its own naturally occurring cannabinoids—the so-called endocannabinoids. They’re involved in the endocannabinoid signaling system, which regulates bodily processes such as stress, mood, social behavior, and pain. The phytocannabinoid CBDV may help soothe ASD symptoms by normalizing endocannabinoid signaling.
“Studies show that individuals with ASD have higher-than-usual levels of circulating endocannabinoids, upsetting the excitation/inhibition balance in neurons by causing too much excitation and too little inhibition,” Dr. Hollander says. “This imbalance can be expressed as meltdowns, aggression, and compulsive or repetitive behaviors.”
Phytocannabinoids can bind to the same receptors as endocannabinoids and appear to restore the balance between excitation and inhibition in neurons. New research suggests that a key component involved in exciting neurons is a lipid called LPI. It binds to a receptor on neurons called GPR55, triggering the release of excitatory neurotransmitters. By binding to and blocking LPI, both CBD and CBDV appear to inhibit the release of these neurotransmitters and thereby dampen neuronal activity.
“It turns out that CBDV is six times more effective at blocking LPI than CBD, which bodes well for our work,” says Dr. Hollander. To explore this mechanism further, Dr. Hollander’s team has launched a study that will measure how CBDV affects a wide range of metabolites, lipids, and endocannabinoids in patients with ASD and PWS.
In a clinical trial involving high-functioning adults with ASD, Dr. Hollander and colleagues are testing a “complex botanical”—a mix of phytocannabinoids plus a low dose of THC, the phytocannabinoid responsible for cannabis’s high. “We’re starting with adults rather than children, since adults will be better able to describe how the drug is affecting their anxiety, mental functioning, and motor coordination,” says Dr. Hollander. “Also, THC can have negative effects on the developing brain. So it’s better to see how the small amounts in our preparation affect key biomarkers in adults before we consider using it on children.”
The challenge now, says Dr. Hollander, is for clinicians and researchers to keep pace with the social and legal acceptance of cannabis that has occurred in recent years. “Certainly the legislation permitting the use of cannabis is much further along when compared with how little we know about its potential benefits,” he says. “There’s a great need for more controlled clinical trials, both for efficacy and for safety.”