
By Gary Goldenberg
Donors and alumni turn a vision into reality with a state-of-the-art surgical simulation center for ophthalmology residents
Anurag Shrivastava, M.D., an associate professor of ophthalmology and visual sciences and the assistant dean for Montefiore Medical Center, winces when he recalls the first time he operated on a living human eye.
He was a junior resident, and although he had observed cases and received a modicum of hands-on classroom training with rudimentary instruments and animal eyes, that preparation hadn’t given him much confidence. Having an experienced surgeon at his side, talking and assisting with each step, kept the patient safe—ultimately allowing Dr. Shrivastava to learn these skills over the course of his training.
“My heart was beating out of my chest,” he remembers. “I was excited, because this was something I’d been waiting to do for years. But it was very stressful—and potentially very dangerous for the patient.”
That first patient did just fine. Years later, however, when Dr. Shrivastava became director of the ophthalmology residency program at Montefiore, he vowed to modernize the way fledgling eye surgeons master their art and craft.
“The conventional approach to learning skills during residency was ‘see one, do one, teach one,’ as the old saying goes,” he says. “That’s an exaggeration, but we did dive right into the operating room with almost no formal training or preparation with simulators. That wasn’t a good approach in ophthalmology because of the complexity of the microscopic surgeries, combined with the extremely small margins of error.”
Even cataract removal—the most commonly performed eye operation—is dauntingly complex. The surgeon must coordinate four different controls (two for the hands and two for the feet) while peering through a microscope and operating on a delicate organ that can’t be completely immobilized. Further complicating the issue, patients, although sedated, are awake during surgery so that they can respond to the surgeon during portions of the procedure. It’s no wonder that Dr. Shrivastava’s first day in surgery was terrifying.
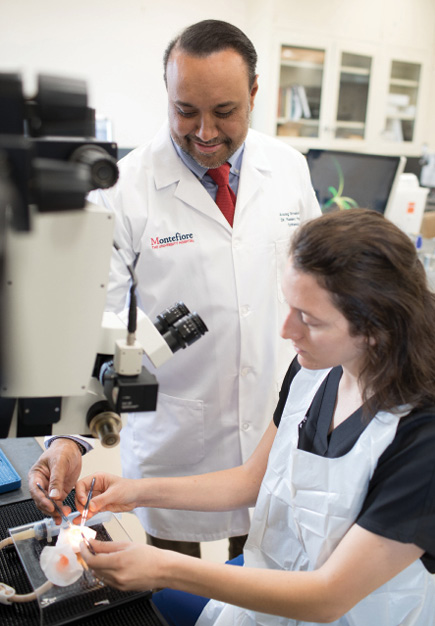 Above: Ana Rubin Panvini, M.D., resident ‘19, practices cataract extraction on an artificial eye with Anurag Shrivastava, M.D. At top of page: Jimmy K. Lee, M.D., Erin Walsh, M.D., Roy Chuck, M.D., Ph.D., and Rob Fargione, M.D., resident '17.
Above: Ana Rubin Panvini, M.D., resident ‘19, practices cataract extraction on an artificial eye with Anurag Shrivastava, M.D. At top of page: Jimmy K. Lee, M.D., Erin Walsh, M.D., Roy Chuck, M.D., Ph.D., and Rob Fargione, M.D., resident '17.
 Members of the Class of 2018 practice intraocular implants. From left are Rachel Shah, M.D., Poonam Misra, M.D., Ryan Gise, M.D., and Isaac Chocron, M.D.
Members of the Class of 2018 practice intraocular implants. From left are Rachel Shah, M.D., Poonam Misra, M.D., Ryan Gise, M.D., and Isaac Chocron, M.D.
 Lectures and group-learning sessions take place in the Ronald M. Burde, M.D., Surgical Simulation Laboratory. At right is Arthur N. Hershaft, member of Albert Einstein College of Medicine’s Board of Trustees and supporter of the ophthalmology department.
Lectures and group-learning sessions take place in the Ronald M. Burde, M.D., Surgical Simulation Laboratory. At right is Arthur N. Hershaft, member of Albert Einstein College of Medicine’s Board of Trustees and supporter of the ophthalmology department.
Dr. Burde’s widow, Sharon, a longtime friend and supporter of the ophthalmology department, has been instrumental in developing the Burde Laboratory, attracting contributions from her husband’s colleagues and from former trainees all over the United States. Says Dr. Chuck: “They look back and realize that it would have been so much better if they didn’t have to learn on patients at the very beginning. Their support is a wonderful gift to the next generation of ophthalmologists, and a fitting legacy to a former department chair.”
Support for the Burde Laboratory has also come from business executive Arthur N. Hershaft. Some 50 years ago, he began experiencing vision loss because of central serous retinopathy, a condition in which fluids collect under the retina. Experimental laser treatments stabilized his eyesight, transforming him into an avid supporter of biomedical research and innovation. A Bronx native now living in Manhattan, Mr. Hershaft has a particular fondness for Einstein, where he has served on the Board of Trustees for more than a decade.
When Mr. Hershaft turned 80, friends asked him where they could make a donation in his honor. “I consulted [then-dean] Allen Spiegel for guidance, and he mentioned the department of ophthalmology,” he says. “I didn’t even know Einstein had such a department. I later learned it conducts a wide range of research and handles 150,000 patient visits a year—one of the largest caseloads in the nation. Few people know what the department is doing and its value to the community. It’s the biggest secret here.”
Mr. Hershaft’s philanthropy and that of his friends and family have helped the Burde Laboratory become an important innovation in medical education. They and their fellow donors have enabled the laboratory to train, teach, and prepare residents for careers in ophthalmology today and far into the future.
“When people ask me why I support Einstein,” Mr. Hershaft says, “I tell them that you can make a real difference here. You can get involved in any number of ways, and the decisions and contributions you make can directly shape the school. There aren’t too many medical institutions where you can have that kind of role.”